We tend to think a typical menstrual cycle runs about 28 to 35 days. Of course, almost all of us have experienced a month or two when our period wasn’t “normal” — during times of extreme stress, heavy dieting or excessive exercise, while taking medications or when we had an illness.

We probably pay more attention to our menstrual cycle at certain times, including when we are trying to get pregnant (or not), or when we’re wondering if we are starting perimenopause.
For all women, the most cycle variability occurs both in the first 5-7 years after their periods start (menarch) and during the last 10 years before cessation of menses (menopause). No matter what your situation, tracking the timeline of your individual menstrual cycle will help you understand your body and identify any irregularities.
Each menstrual cycle naturally requires the rise and fall of certain hormones — estrogen, progesterone, and two pituitary hormones known as follicle stimulating hormone (FSH) and luteinizing hormone (LH). Though coordination between these hormones varies for each of us, the general sequence follows a basic pattern. If this pattern is disrupted frequently, it can be a sign of hormonal imbalance and a clear message that your body needs more support.
Hormonal changes throughout the menstrual cycle
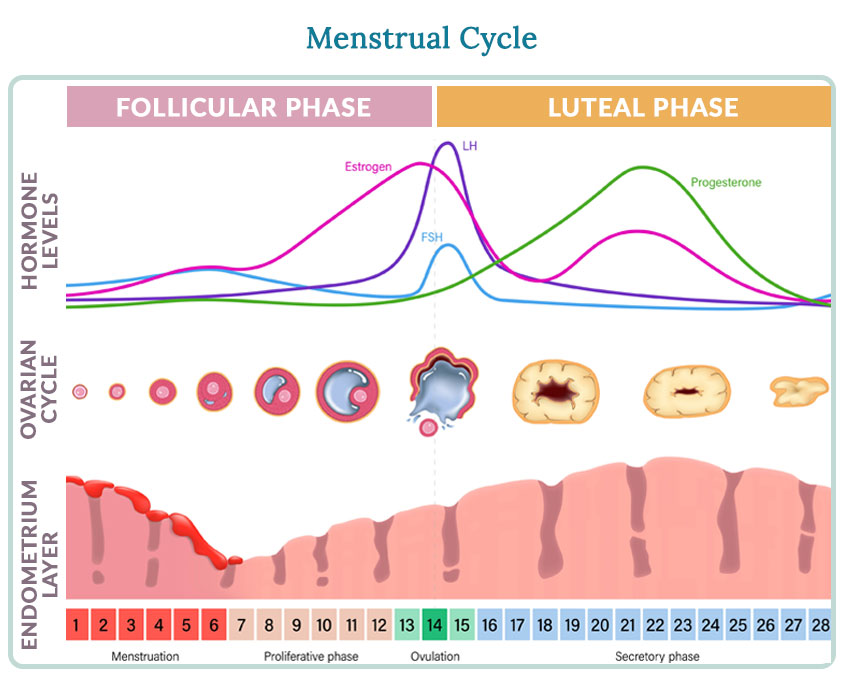
As shown in the chart, changes our pituitary hormones, uterine lining, egg development and ovarian hormones take place throughout our cycle. With day 1 as the first day of menstruation, here is a textbook 28-day example of what happens:
Days 1-14 (the follicular phase): Estrogen levels rise as your body prepares an egg for release. Just before ovulation, your hypothalamus and pituitary gland release hormones to trigger ovulation. Any changes to the duration of your cycle are due to alterations in this phase.
Around day 14: Ovulation. Generally, you’re most likely to get pregnant during the two to three days around the time you ovulate.
Days 14-28 (the luteal phase): After you ovulate, your estrogen levels begin to decline. Progesterone levels begin to increase. This phase is relatively constant.

What if my cycle doesn’t feel normal? How PMS and perimenopause figure in
You may wonder why we didn’t include the “PMS phase” in the textbook menstrual cycle above. Many women are so used to dealing with irregular periods, cramps, irritability and bloating that they assume PMS is part of a normal menstrual cycle. It’s not. PMS is caused by disruptions of the natural rhythm of our hormones, and these can be triggered by everything from food choices to stress responses to activity levels.
Perimenopause is another time when hormonal imbalance can upset your regular cycle. Changing or unpredictable menstrual cycles may be the first perimenopause symptom a woman notices. It’s a good opportunity to begin providing extra support right away to help prevent additional symptoms including hot flashes, irritability and weight gain. Waiting until it gets worse is not an effective strategy.
Getting back to your natural menstrual cycle
After working with thousands of women, we’ve seen how much better women can feel when they follow the natural approach to finding hormonal balance in our Women’s Health Network Hormonal Health Programs. Available in several versions, this targeted approach helps maintain your regular menstrual cycle, and can help guide your body back on track if you’re suffering from PMS, perimenopause or another hormonal imbalance that’s affecting your cycle.
When your body has what it needs every day— the right nutrients, consistent stress relief and self-care —it has the power to heal itself so you can feel your best.
* Adapted from information at McGill University and the University of Wisconsin.









