Conventional medicine has been battling heart disease for decades with major therapies, surgery and prescription drugs that are not preventative and arguably are ineffective. At Women’s Health Network, our approach to heart health focuses on preventing heart disease and related conditions. And conventional medicine is starting to catch on. The historical development of heart disease in America and research developments help explain why we advocate a holistic approach.
What is cardiovascular disease?
Heart disease, hypertension and stroke are cardiovascular conditions, meaning they involve your heart and arteries. Damage is caused when the heart muscle weakens or dies because of infection or reduced blood flow. Stroke occurs when the blood vessels leading to the brain are blocked or constricted. Both are commonly the result of a build-up of arterial plaque (atherosclerosis). High blood pressure, or hypertension, also results from the narrowing and hardening of the arteries caused by atherosclerosis.
Read our list of the most common cardiovascular diseases and conditions.
Cardiovascular disease is most common in industrialized countries where modern lifestyles include the worst risk factors: smoking, obesity, lack of physical activity, high cholesterol, and inflammation. Heart disease seems so simple that it should be preventable. Then why does heart disease affect more than 500,000 women a year?

Heart disease is not the same for women
Heart disease is the leading cause of death for American women. Yet, in a recent study, fewer than one in five physicians recognized that more women than men die of heart disease each year. This cultural gender bias perpetuates the myth that heart disease is a “man’s problem” and that threatens the health of all women.
The reality is that, while mortality rates for men over the past 20 years have declined steadily, the rates for women have remained relatively stable. Part of the reason this misperception is so prevalent is because the symptoms of heart disease are different in women. Many doctors may not even recognize them until a major cardiac event is taking place which means that women may receive less aggressive treatment, and occasionally no treatment at all. (See our list of warning signs of heart attack and stroke)
One problem is that many physicians use the same risk assessment tools for both men and women (e.g., the Framingham Risk Estimation [FRE]). This practice fails to identify a significant number of female patients who already have coronary disease.
On top of that, most women aren’t informed about heart disease prevention without a prior diagnosis or family history even though there is a universal risk posed by menopause when levels of “good” cholesterol drop. That means that women are often misinformed, misdiagnosed, and compromised in terms of their heart health. In addition, the majority of studies on heart disease have been conducted on a white male population, with women mostly left out of the picture.
Women and the history of heart disease
Medicine has approached heart disease as an evil threat created by one villain after another. Doctors began diagnosing men with symptoms of cardiovascular disease as early as the 1930’s. After World War II, our farm-based society evolved into an urban/industrial society, with a distinct shift to a life of relative wealth, abundant food, and physical ease. And we became victims of our own prosperity and good fortune.
We began eating too much, driving instead of walking everywhere, working at desks for hours on end, and smoking and drinking to excess. The new stressors of modern life multiplied, along with environmental pollution. These factors led to some people’s arteries reacting by creating sticky plaque that, among other things, constricted blood flow to the heart and other organs and weakened them.
By the late 1940’s, heart disease was officially proclaimed the number one killer, though statistics on women from that time don’t exist. Doctors blamed the condition on an overly rich diet — much the same as gout — because a majority of the men who had it were overweight. In the 1950’s doctors learned that smoking was a huge risk factor, but cigarette makers kept this information from the public.

Twenty years later, the government got involved and huge amounts of funding went towards finding causes and a cure. In 1971, the US Public Health Service underwrote the landmark Framingham Heart Study. This ongoing study, the first to include women, is the basis for much of what we know about heart disease today. And — for the first time ever — it verified the link between cardiovascular disease and our lifestyle, or what came to be known as “heart disease risk factors.”
New information in the 1970’s identified stress and the “type–A personality” as factors. Then in the 1980’s, we discovered the link with saturated fat and cholesterol and ushered in the ineffective low-fat craze of eating.
In the 1990’s we discovered “good” and “bad” cholesterol. Now, current research points to inflammation as the chief assailant to our heart health. Our guess is that individual DNA variations will move to the forefront in the near future as genetic profiling improves. If the cause of heart disease were a multiple-choice question, the answer would be “all of the above.” And more.
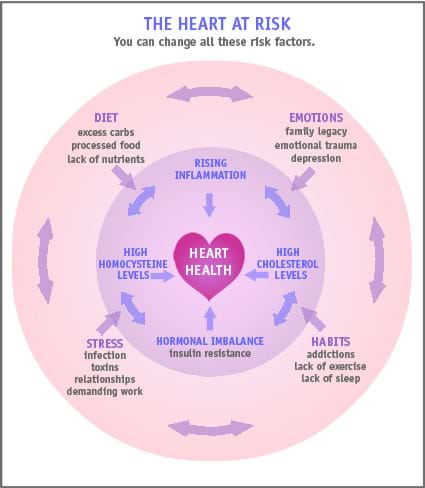
There’s more than one villain with heart disease
The danger of the “villain” approach we’re used to with heart disease is that it oversimplifies the problem, and leaves out the great potential of prevention. Western medicine already mostly waits until the patient reaches a disease state, before diagnosing and treating aggressively. This wait-then-intervene approach may save your life once you’re really sick, but isn’t effective at preventing the problem in the first place, when it’s so much easier to address.
Surgical solutions like heart bypass surgery (which “fixes” a blockage by “bypassing” it) and arterial stents may be crucial for people with advanced heart disease. But they still tend to “buy time” without getting at the underlying cause of the disease.
Similarly, statins (Lipitor, Zocor, Pravachol, Lescol, Mevacor) may lower cholesterol, but lead women to rely on a drug to manage effects, rather than getting at what drove up their cholesterol in the first place. Most important, statins are not magic potions but powerful drugs — with powerful, and sometimes debilitating, side effects such as muscle pain and depletion of co-enzyme Q 10, a key nutrient we need to make energy. The truth is we don’t know all the long-term implications of statin use.
We know that sometimes high cholesterol is correlated with cardiovascular disease risk, but that doesn’t mean it causes it. A majority of heart attack sufferers have normal cholesterol readings. And the supposed cause-and-effect link between high cholesterol and heart disease has never been proven in the first place.
All this led to low-fat diets which effectively starve the body of the nutrients it needs. Low fat diets overlook the negative side effects, and have created an epidemic of insulin resistance, which, ironically, new studies show is a clear risk factor for heart disease.
Heart disease prevention — a better understanding
Still, we have learned a lot about the heart, and more cardiologists are realizing that there’s no simple answer: heart disease is multifactorial and is best treated by identifying and reversing the underlying problems.

There have been many important findings from studies of heart disease in recent years:
- Inflammation is a critical risk factor — perhaps more important than cholesterol — which means that heart health is related to all the other systems of the body, from nutrition to dental health to digestion to hormonal balance to heavy metal toxicity.
- High blood sugar, whether you are diabetic or not, also appears to raise the risk of heart disease.
- The connections to depression and stress are clearer and stronger and the role of emotional experience is getting greater recognition.
It’s proven beyond any doubt that synthetic hormones raise the risk of cardiovascular disease. We don’t know yet but hope that bioidentical hormones may actually reduce it.
- The risk factors for heart disease reach far back into our personal history.
- The genetic factors play a smaller role than we may at first have feared.
Steps you can take right away to support heart health
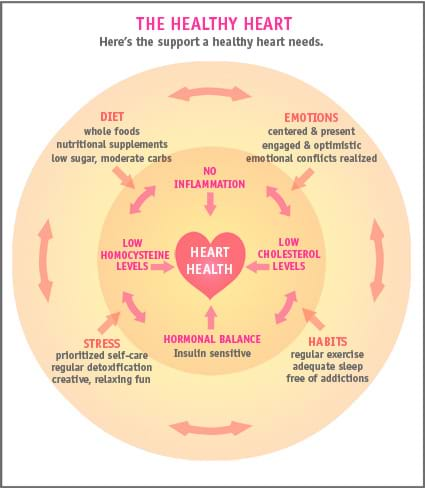
At Women’s Health Network we are so encouraged by these developments. We now see conventional medicine backing into an understanding of heart health that is profoundly holistic: everything in our lives is connected and our mind, body and spirit each play roles in determining our health. We finally understand that nature is the real healer and prevention is more effective than treatment.
What can you do right now to help your heart stay as healthy as possible?
Consider taking these two steps:
1. Supplement every day with high quality fish oil, in the same dosages as supported by research. Choose a fish oil with both EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) that totals about 1000mg, or one gram.
2. Add coQ10 — choose a supplement that provides 100mg every day
Visit a functional medicine practitioner for further information about your individual needs. You’ll find additional guidance on holistic heart health when you read about our approach to natural heart disease prevention.
URL: https://www.docguide.com/news/content.nsf/news/
https://www.docguide.com/news/content.nsf/news/8525697700573E18852570D9004C7B5E (accessed 01.04.06)
Michos, E., et al. 2005. Women with a low Framingham risk score and a family history of premature coronary heart disease have a high prevalence of subclinical coronary atherosclerosis. AHJ, 150 (6), 1276–1281.